Customer:
Statement Scrubber
Industry:
Revenue Cyle Management
Website:
Product Used:
Autymate Statement Scrubber


Autymate helped us to identify, define, document, improve, integrate, and deliver all ecosystem procedural components in a single visually and operationally consumable web portal containing actional RCM KPI data.
In this case study, this medical group was searching for ways to improve the way they manage patient billing and reduce incoming calls because of client billing issues. The "Autymate | Statement Scrubber" application reduced the medical group's statements and costs by 50% by over $11,000 and anticipate it to reach a reduction of over $15,000 by year-end (2019). We successfully eliminate incoming calls related to in-accurate balances, capture un-filed charges cycle after cycle, and help to extract all 120+ days of aged accounts.
About
Background
The practice administrator of a southeastern primary care & multi-specialty group was searching for a way to stop the “ill-will” phone calls coming into their billing call center.
The calls were triggered by patients receiving an erroneous balance due on their statements because it did not reflect all payments made to the office. The practice needed an easier way to capture these unapplied credits before the statement files were transmitted to their statement service vendor.
There was an added concern for their ever-increasing monthly statement count. The opportunity to have light shed on the reasons for the escalating cost of statements was of great interest to them.
The Challenge
This clinic was operating on the Greenway Prime Suite EMR/PM system. The weakness of the system is its inability to keep patient payments and credits linked to the appropriate patient charges and balances. The billing team was required to run daily reports to identify patients with credits so that they could get them applied to balances before the statements ran each night. It was not only a daunting task but also an imperfect workflow causing statements to prematurely be released for mailing. This process typically took one staff member 30 to 45 minutes each day to perform. The phone call volume averaged over 240 per month (12 calls per day).
Similarly, the Prime Suite system does not offer an automated feature to prevent sending patient statements incessantly. The billing team relied upon a manual process to try to stay ahead of accounts that are aged and/or patients–particularly the uninsured–that were failing to pay their balances or maintain payment plans.
Our Solution
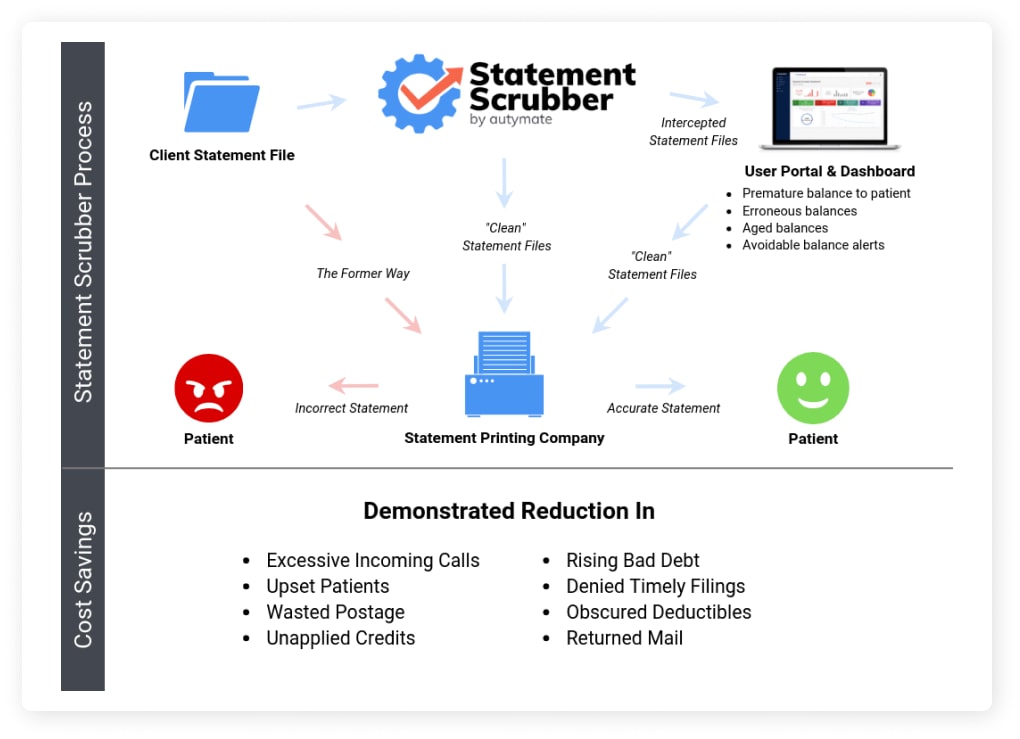
Utilizing the Statement Scrubber (the “Scrubber”) application, the practice was able to securely submit their statement file through the Scrubber on a bi-weekly basis for its automated previewing functions. Each incoming file was scrubbed for statements containing overstated balances. They were identified, suppressed, and reported back to the practice. The “clean” statements were then forwarded to the statement service provider for normal processing and delivery.
The Scrubber also identified a high volume of accounts that had aged beyond 120+ days. The suppression action was applied based on built-in Best Practice criteria while the less-aged accounts were allowed to pass through for mailing. The RCM director was able to access the Scrubber user portal to work through each of the outstanding balances using the sort & filter options provided. In addition, they were able to establish a “new normal” within their billing department using more manageable workflow processes.
Performance Outcome
▪ 0% reduction in statement volume and cost compared to same time period in previous year
▪ Over $11,725.00 saved in statement cost in 8 months
▪ A near complete elimination of incoming calls relating to unapplied credits
▪ Earlier capture of aging balances & repetitious billing
▪ Bad debt reduction associated with untimely claim-files or appeals
▪ Additional revenue leaks & opportunities identified i.e. copay shortages & outdated payment plans
Bottomline
By utilizing the Autymate | Statement Scrubber application, this medical group was able to significantly improve their patient billing processes and reduce incoming calls related to inaccurate balances. The Scrubber automated the previewing of statement files, identifying and suppressing statements with overstated balances and reporting them back to the practice. As a result, the medical group was able to reduce their statements and costs by 50%, saving over $11,000 in just 8 months, and anticipate even greater savings by year-end.
The Scrubber also allowed the medical group to identify a high volume of accounts that had aged beyond 120+ days and establish a "new normal" within their billing department using more manageable workflow processes. With the Scrubber's powerful sorting and filtering options, the medical group was able to work through outstanding balances more efficiently and reduce bad debt associated with untimely claim-files or appeals.
If your medical group is struggling with patient billing processes and seeking ways to reduce costs and improve efficiency, consider partnering with Autymate and leveraging our Statement Scrubber application.
Set up a Whiteboard Session with us HERE, and our custom solution can help your medical group improve patient satisfaction and financial performance.